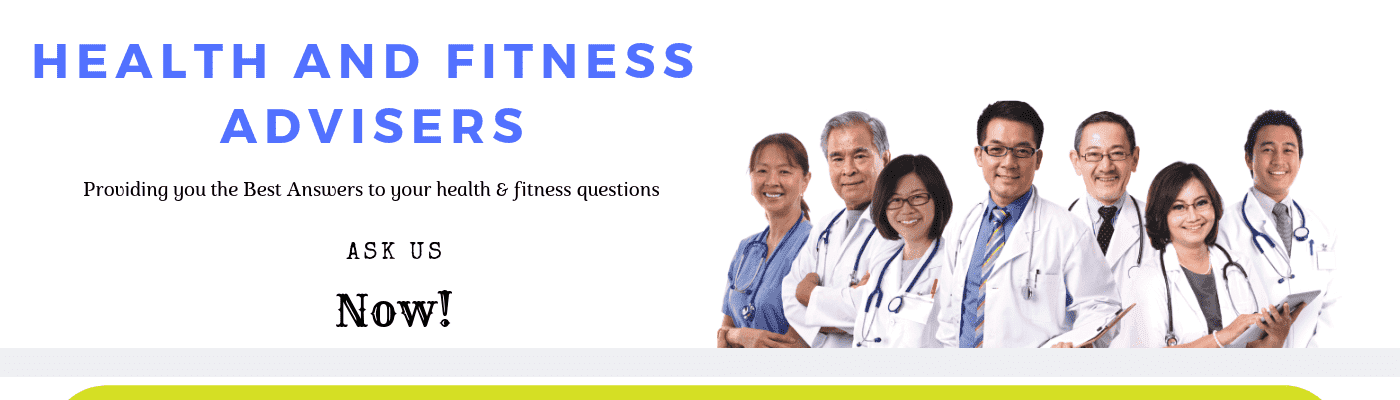
The two diseases may be so similar that some people don’t recognize the difference.
But the truth is that not all of their symptoms are the same.
Vulvovaginitis vs Yeast infection are very similar in many ways, but there are some key differences.
Yeast infection symptoms like pain and itching usually come and go, whereas Vulvovaginitis symptoms tend to linger.
The vulvovaginitis infection also has the potential to become an STD or sexually transmitted disease.
Women who have vulvovaginitis can contract a number of STDs, including Chlamydia, gonorrhea, and herpes.
Vulvovaginitis is not the only condition that can cause symptoms similar to those of a yeast infection.
Genital yeast infections are increasing among both men and women.
Table of Contents
Vulvovaginitis vs Yeast Infection: Symptoms & Treatment Needed
A yeast infection caused by bacteria can be quite serious, but a yeast infection caused by a virus can be deadly.
Likewise, a vaginal infection is caused by a fungus or mold that grows and feeds on the body’s sugar.
Also, a yeast infection is caused by the same fungi, but it has a protein coat that prevents it from being destroyed by the body’s immune system.
When the body’s immune system attacks this coating, it can lead to an infection.
In fact, vulvovaginitis and candida are caused by the same types of bacteria.
However, while candida causes an infection, vulvovaginitis is more of an irritation.
This is because the vulvar area in women is particularly sensitive and vulvovaginitis can come from using certain antibiotics.
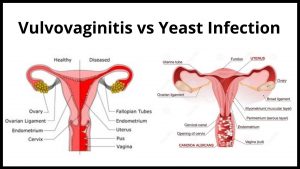
In fact, one of the main symptoms of vulvovaginitis is a thickening or cracking of the vaginal walls.
In addition to these symptoms, you may also experience a white-ish discharge from your vagina that has a foamy texture.
Knowing what are the differences between vulvovaginitis and yeast infection will help you determine if you need medical treatment for vulvovaginitis or not.
A yeast infection often occurs on the outer layers of skin, but it can be found under the surface of the vagina as well.
Also, yeast infection commonly occurs in the mouth.
There are several things that set apart vulvovaginitis from a simple yeast infection.
First of all, vulvovaginitis often causes symptoms such as itching, burning, redness, and swelling around the vulva.
These symptoms do not go away no matter how much of a treatment you take.
In addition to the itchiness, burning, and swelling, vulvovaginitis often causes pain during sexual intercourse.
Knowing what are the differences between vulvovaginitis and yeast infection will help you determine if you need medical treatment for vulvovaginitis or not.
There are several things that set apart vulvovaginitis from a simple yeast infection.
First of all, vulvovaginitis is usually persistent over time and doesn’t clear up within a few days to a week.
In addition to this, vulvovaginitis can cause pain during sex, itching, and swelling around the vulva.
As you can see, these are all pretty much the same symptoms as a yeast infection, but one is a little more annoying than the other.
Yeast infections are generally considered to be more serious conditions and should be treated by a medical professional.
While it can be uncomfortable to have a yeast infection, the discomfort usually passes fairly quickly, as long as you are careful about cleaning and drying your genital area thoroughly after cleaning.
You can avoid contracting vulvovaginitis if you are careful about following proper preventative measures.
Such as maintaining a healthy vaginal environment, staying away from cigarette smoke, keeping up with any vaccinations that you may need to keep yourself protected.
And using any over-the-counter medications recommended by the doctor.
Vulvovaginitis – Tips for identification.
Vulvovaginitis is an inflammation or irritation of the vulva, which is the genital area’s lining.
Common symptoms of vulvovaginitis are burning, itching, and swelling.
In addition, a vulvovaginitis infection often affects the vaginal area while a yeast infection is more likely to affect the skin surrounding the vagina.
There are other vulvovaginitis cases that do not have any external symptoms.
However, when vulvovaginitis does occur it usually comes in the form of redness, swelling, and pain.
There are many things that can cause vulvovaginitis.
It can be caused by a change in vaginal detergent, dry skin, and/or sex.
Vulvovaginitis can also be caused by a decrease in estrogen.
However, the most common cause of vulvovaginitis is a yeast infection.
A yeast infection can cause a wide range of symptoms including painful intercourse, itching, and discharge.
Treatments for vulvovaginitis vary.
Just like treating a yeast infection, you will want to use a neutral pH vaginal lubricant, such as baby oil or natural yogurt.
You should also treat your vulvovaginitis with a weak douche so that you are not adding too much extra acid to the vagina.
Also, you should be using light cotton underwear and a short-sleeved, dry and clean shirt.
For vulvovaginitis that doesn’t seem to respond well to over-the-counter treatments, you may want to look into prescription medications or antibiotics.
These are usually reserved for cases where vulvovaginitis is severely recurring or has caused damage to the skin.
Unfortunately, since this is often the case with vulvovaginitis that doesn’t respond well to normal treatment methods, many doctors will recommend a visit to the doctor to ensure the infection is actually vulvovaginitis.
And not a more serious condition.
Common treatments for vulvovaginitis include topical creams, antibiotics, and anti-fungal suppositories.
Some experts even advise adding a small amount of yogurt to the vaginal area to help alleviate the discomfort.
These methods should only be used as a temporary solution for vulvovaginitis.
As soon as vulvovaginitis has been identified, it should be treated immediately.
Women who have vulvovaginitis are encouraged to practice strict preventative measures so that they do not develop the infection often.
This includes keeping the vaginal area clean and dry.
Also, this helps to prevent the development of fungal bacteria and keeps the vagina healthy.
In addition, treatment for vulvovaginitis can be taken orally or sublingually.
The choice of treatment should be made based on the diagnosis of vulvovaginitis.
If you choose to treat your infection with oral medication, make sure that it is anti-fungal and taken according to schedule.
In addition, if you choose to treat your infection with a suppository, it should be inserted in the same way it was meant to be inserted.
To relieve symptoms of vulvovaginitis, many women turn to alternative treatments such as homeopathic medicines.
Homeopathic medicines are very effective in treating the symptoms of vulvovaginitis, but not always effective at curing the infection.
This is because some homeopathic medicines are geared towards healing the symptoms of yeast infection while not curing vulvovaginitis.
For this reason, it is not uncommon for many women to experience recurrent vulvovaginitis.
Therefore, when deciding which treatment to use for vulvovaginitis infection, it is important to carefully consider both the symptoms and the cause of vulvovaginitis before choosing a treatment.
In conclusion, vulvovaginitis is characterized by redness, swelling, and irritation in the vulva area.
It is a common infection that is often mistaken for a yeast infection.
Although vulvovaginitis can be very irritating, if left untreated, it can lead to chronic yeast infection.
Therefore, if you choose to use a natural treatment for vulvovaginitis.
Be sure to take into consideration both vulvovaginitis and yeast infections to determine which treatment would be best for you.
If vulvovaginitis is the primary infection, it is important to address both issues at once.
Some treatments such as yogurt, vinegar, and acidophilus can be very effective at treating the symptoms of vulvovaginitis and also at curing the infection.
These treatments can be used on their own or when added to other remedies such as tea tree oil.
However, if the vulvovaginitis is caused by a secondary infection, these same treatments will not be as effective.
When deciding which treatment option to use for vulvovaginitis a yeast infection, it is important to be educated about the symptoms of vulvovaginitis.
Know the signs and symptoms of vulvovaginitis so you can immediately identify if you have vulvovaginitis.
Next, learn about the different vulvovaginitis treatments.
Finally, learn about the underlying causes of vulvovaginitis.
Once you have identified these causes, you can choose a treatment option that will work best for you.
If vulvovaginitis is not the primary condition causing your symptoms, don’t be afraid to take conventional treatments such as over-the-counter medications and creams.
These are effective for many women.
If, however, your vulvovaginitis is caused by a more serious underlying condition like a yeast infection.
You may want to consider a more specialized approach such as a completely natural, alternative approach to curing both conditions.
The natural approach takes into account vulvovaginitis treatment that addresses both the underlying cause and symptoms of vulvovaginitis.
This is by far the most effective approach to curing vulvovaginitis.
Yeast Infection – Tips for identification.
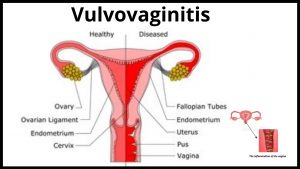
A yeast infection, also known as vaginal candidiasis, occurs when the naturally occurring yeast that resides in the vagina gets out of control.
It may result in itching and other uncomfortable symptoms.
Candida albicans is the organism responsible for causing a yeast infection.
Some of the more common causes and types of this condition include:
Vulva:
Women who are pregnant sometimes suffer from a vulva yeast infection.
The vulva is the skin surrounding the vulva, the inner portion of the female genital organ.
It is very tender and red and can become irritated when trapped between garments.
Abnormal white or red discharge, itchiness, and pain in the vulva are some of the symptoms associated with a vulva yeast infection.
Other symptoms include pain during intercourse and burning while urinating.
Vagina:
A woman may have a vaginal yeast infection if she has unprotected sex with a man who is a carrier of the organism.
Women who douche may also have an abnormal discharge.
Also, women who wear tight-fitting underwear may find that they can develop skin lesions.
Untreated infections in the vagina can result in thickening and puffing of the tissues there.
Imbalance of Body System:
Certain imbalances in the body can lead to an imbalance in the body’s natural defenses.
This can lead to the occurrence of yeast infections.
A woman’s immune system can become deficient due to various factors including illness, overuse of antibiotics, and exposure to certain chemicals.
These factors can weaken the vagina’s natural defenses and allow Candida albicans to multiply and grow out of control, resulting in an infection.
Many medications that are used to treat other conditions, such as high blood pressure, cancer, cysts on the ovaries, and others, can actually increase the level of Candida albicans in the vagina.
Taking these medications without addressing the underlying issues can make the condition worse.
Risk Factors:
The vagina is one of the least preferred and easiest places in the body to establish an infection because it is dark, private, and closed off from the rest of the body.
Yeast infection in this area is most often found in women who take antibiotics for long periods of time or women with poor immune systems.
Women who douche regularly may increase the risk factors for candida infections.
Other risk factors include diabetes, which increases blood glucose levels; AIDS/HIV, which decreases the resistance against infection; pregnancy, which exposes the vagina to an unusual environment that may increase the risk factors for yeast infection.
And birth-control control pills, which alter the normal environment of the vagina and change hormonal levels.
Treatment Options:
Most people choose an over-the-counter medication to treat their condition.
These are typically topical creams or pessaries that contain the antifungal agent clotrimazole, although fluconazole is sometimes added.
Some prescription medications do not contain clotrimazole and contain miconazole instead.
Popular creams and lotions used as a topical treatment contain ketoconazole, antifungal nystatin, or amphotericin B, and act as an anti-fungal and anti-vaginal discharge thickener.
For more intense itching or burning, it may be necessary to use prescription steroids, oral or topical antibiotics, or other potent prescription medicines that act as a broad-spectrum antibiotic.
In cases where the over-the-counter medications fail to provide relief, or if severe symptoms persist, a doctor should be consulted.

How Is Vulvovaginitis Diagnosed?
Vulvovaginitis is inflammation of the vulva, which is a mucous membrane that lines the genital organs.
The symptoms of vulvovaginitis are usually itching, burning, redness, and thickening of the vulva skin.
These may appear on any portion of the vulva but are most often seen in and around the vaginal opening.
If you do not start an appropriate vulvovaginitis treatment protocol at the right time, then you may suffer more serious vulvovaginitis later on down the road.
For this reason, it is important to learn how to correctly diagnose vulvovaginitis, so that you can begin to treat it immediately.
When you are looking for a vulvovaginitis diagnosis, you have several options available.
A doctor may order a vulvovaginitis sample from your vulva to be tested for viral cultures.
They may take a scraping from the vulva to look for signs of infection or to simply look for inflammation.
Vulvovaginitis diagnosis refers to the presence of at least four signs and symptoms of vulvovaginitis.
The vulvovaginitis diagnosis used will depend on the area of the vulva that is affected, the symptoms experienced, and how detailed a patient’s medical history is.
Vulvovaginitis is usually caused by an infection of the vulva, although other causes have been described including yeast or fungal infections.
Also, vulvovaginitis is most commonly caused by staph bacteria.
Vulvovaginitis diagnosis can be confirmed if doctors find a specific bacteria present in the vulva.
This means that staph is easily kept in check with antibiotics.
In many cases, vulvovaginitis infections are not accompanied by any other symptoms.
The only way to determine if a patient has vulvovaginitis is by performing a routine physical examination.
The exam includes a query about the woman’s recent history and symptoms that may be associated with vulvovaginitis infections.
A doctor’s professional training and experience in the field will help determine the correct vulvovaginitis diagnosis.
Vulvovaginitis can have multiple causes.
It can be caused by fungal or viral infections.
An indicator of vulvovaginitis would be a yellow-green discharge from the vagina.
Vulvovaginitis diagnosis can also be confirmed by performing culture of the discharge.
Although not a foolproof test for all cases of vulvovaginitis, a sample of the discharge can help doctors confirm an infection.
If a patient continues to have a yellow-green discharge despite a visit to the doctor, vulvovaginitis diagnosis is almost certainly confirmed.
If a discharge is not present, but the other symptoms are present, this can also be used as an indicator of vulvovaginitis.
These include fever, swelling of the legs, and itching or burning in the vaginal area.
Vulvovaginitis diagnosis can be affected by factors in a patient’s environment.
For example, if a patient spends a lot of time around an industrial facility where fecal bacteria may be common, they may be at greater risk of developing vulvovaginitis.
This is also why it is so important to keep one’s hands and vagina clean and dry at all times.
It can be especially dangerous during menstruation when spotting and possible vulvovaginitis are more likely.
In addition to keeping yourself healthy, you should take care to avoid wearing tight-fitting pants, pantyhose, or any other clothing that might irritate your skin.
Vulvovaginitis diagnosis may also be affected by one’s age.
Younger women can generally rest assured that their vulvovaginitis diagnosis will be positive.
The reason for this is that young women are more likely to be affected with bacterial vaginosis than older women.
The same can be said for women who are obese.
Finally, women who douche can also expect a negative vulvovaginitis diagnosis.
These factors can all work together to create a positive diagnosis and hopefully a treatment option as well.
Once vulvovaginitis diagnosis has been received, the doctor will then discuss the treatment options open to them.
While some patients will opt to use prescription medications, others may want to try a natural remedy first.
In fact, most patients these days are opting to use a natural remedy to treat their vulvovaginitis.
There are many different options available that a patient may want to consider.
The important thing is to remember that with vulvovaginitis diagnosis, there are several treatment options that your doctor may recommend.

How Is Yeast Infection Diagnosed?
Vaginal candidiasis can be self-diagnosed with the use of over-the-counter medications available at most pharmacies.
Women who suspect that they have VVC should see their doctor immediately since these over-the-counter medications cannot get to the root cause of the problem.
For serious cases, VVC may require surgery to remove the smelly patches of skin.
Treatments for VVC include amoxicillin, clotrimazole, and miconazole.
Another way to self-diagnose vaginal yeast infections is to purchase over-the-counter medications at your drugstore.
You can find an abundance of products at your drugstore.
One popular brand is Monistat, which is easy to use and highly effective in treating female (vaginal) candida.
Other popular brands of over-the-counter medications for vaginal infections include Clotrimazole, Butoconazole, and Tioconazole.
However, you should be aware that these medications do not cure vaginal infections.
They simply treat the symptoms.
In order to confirm the diagnosis for vaginal yeast infections, a doctor may take a scraping from inside the vagina to look for the presence of candida.
The doctor may take samples of the vaginal discharge and perform a culture to confirm the existence of candida.
Also, the scraping is usually done in a lab, but some doctors perform this test at home.
Samples of the vaginal discharge will usually show signs of both yeast and candida.
A doctor may take a sample of the vaginal discharge and send it to a laboratory for further testing.
There are several laboratory tests that can confirm the diagnosis for vaginal yeast infections.
– Miconazole can be used to confirm the diagnosis of vaginal yeast infection.
Monistat, however, may not work effectively in women who are taking oral contraceptives.
Oral contraceptives prevent the vaginal dryness that causes vaginal yeast infections, so they can increase the likelihood of developing a vaginal yeast infection.
– A blood test may be performed to confirm the diagnosis for vaginal yeast infections.
A doctor may take a sample of vaginal discharge or excreta, to check for the presence of candida.
The pH level of the discharge may be checked to determine whether or not it contains a high level of glycogen, which is created by the candida for fuel.
The doctor may also examine vaginal fluids for the presence of sperm.
If there is no sperm, and the vaginal yeast infection is caused by candida, then the condition can be treated.
– A culture of vaginal discharge from a woman who is suffering from a vaginal yeast infection can be sent to a lab for testing.
The doctor will look for the existence of candida in the vaginal discharge.
This test will likely require two separate samples of vaginal discharge.
One sample will be taken without the use of a douche, while another sample will be taken with a douche.
– Another way to confirm the correct diagnosis for vaginal yeast infections is to look at the condition of one’s vagina.
If you notice any discoloration or sores in your vagina, they may be signs that you have one of these infections.
Your vagina should be smooth and moist.
There should not be an abundance of discharge either.

How Is Vulvovaginitis Treated?
Many women suffer from vulvovaginitis, a painful and itchy infection of the vulva, which is the lower part of the vagina.
Vulvovaginitis is more common in women who are over 50 years old.
The vulva can become irritated and inflamed due to different factors such as sexual abuse, hygiene, or allergies.
Vulvovaginitis treatment is one way to reduce the itchiness, burning sensation, and inflammation caused by the infection.
There are many treatments available for vulvovaginitis.
Some of the methods are conventional medication such as antibiotics or creams, while others can be more unconventional such as acupuncture, herbal, and homeopathic remedies.
Your doctor can prescribe medications and recommend a vulvovaginitis treatment method based on the cause of your condition.
There are many natural treatments for vulvovaginitis.
Herbal supplements and teas that can be used to help alleviate symptoms are quite effective in soothing the vagina.
And are strengthening the immune system to fight off the infection.
These treatments are safe and effective for most women.
There are some, however, who should not take herbal treatments because some have been known to cause an allergic reaction or cause stomachache, nausea, or gas.
Another effective method of treatment is the use of topical creams.
These have no side effects and can be applied several times a day to relieve the itching and burning.
Over-the-counter topical treatments containing anti-fungal agents can also be used to treat vulvovaginitis.
Most of these treatments contain ingredients that will not only relieve the irritation but will also stop the growth of fungus.
However, if the infection is still present, it is best to consult a doctor to make sure that the treatment you are using is the right one for your condition.
In more serious cases of vulvovaginitis, antibiotics may be prescribed by the doctor.
It is important to realize that antibiotics can only be prescribed after a bacterial culture test has been performed to see if your condition is actually caused by a bacterial infection.
Antibiotics are often used for cases where vulvovaginitis is considered to be at a severe level.
A bacterial infection causes the most common complications of vulvovaginitis and includes swelling and redness, painful sexual intercourse, and itching.
Although these symptoms can be alarming, they are usually caused by bacterial infections and do not warrant the use of antibiotics.
Surgical procedures such as vulvovaginitis implants have become a common way of how is vulvovaginitis treated.
Unfortunately, surgical treatments should only be considered as a last resort once medical examinations have ruled out other options.
The use of lasers, laser ablation, and excision have also shown to be effective in the treatment of vulvovaginitis.
But due to their potential side effects, they should only be used as a temporary measure.
Over-the-counter treatments are available for vulvovaginitis range from simple moisturizers and acidophilus powders to more drastic treatments available for vaginal infections.
These treatments can range from being purely symptomatic to being invasive and complicated.
As with all ailments, it is always best to seek medical advice before deciding which route to take in your search for how is vulvovaginitis treated.
A healthy vagina is a perfect environment for healthy bacteria to thrive, however for those with vulvovaginitis this is not the case.
Vulvovaginitis is caused by an imbalance of the pH levels within the vagina.
This can be treated using simple douches made of plain water and tea tree oil or even apple cider vinegar with water.
Natural remedies may also be the answer when it comes to treating the condition; however, it is important to remember that vulvovaginitis is an infectious disease and should be treated as such.

How Is A Yeast Infection Treated?
There are many treatments out there, but before you go any further with any of them, I would like to tell you about my preferred method of treatment.
Natural yeast infection treatment.
This involves a change in diet and lifestyle, which includes drinking plenty of water, staying away from sugar, alcohol, and coffee.
As these products can encourage the growth of the fungus and can create additional discomfort, it is highly recommended that you avoid them as much as possible.
The first step in any yeast infection treatment method is to make sure you have a healthy immune system.
This means you have to drink plenty of fluids especially water.
You also need to get plenty of rest.
It is a common misconception that people with sickly immune systems are more prone to Candidiasis.
On the contrary, healthy people are prone to it too.
Once you have cleared up your immune system, the next thing you need to do is to get rid of the internal bacteria or fungi that are causing the infection.
You can take antibiotics but these may have side effects, and these cannot always prevent the occurrence of yeast infections.
Antibiotics can kill other helpful bacteria in our body such as the acidophilus bacteria.
Acidophilus is a good bacteria that help keep yeast infections at bay.
Another important thing to know about yeast infections is that the best treatment is to kill the fungus.
To do this, you can either use topical creams that cure the condition or take pills that are ingested.
Some women prefer to apply the cream to their affected area while others opt to take oral tablets.
Although this method does not guarantee a complete cure, it can be quite effective.
The anti-fungal drug that is most commonly prescribed is Monistat which contains clotrimazole, which is also used to treat other types of infections.
Yeast infection will not go away unless you address its root cause.
Many women resort to over-the-counter medications which can have harmful side effects.
For women who have just gotten over their previous infection, they may think that it will go away on its own.
However, the infection will never completely go away unless you address its causes.
Once you finish with your treatments, the infection will just keep coming back until you get a thorough cleaning from a health practitioner.
This may sound discouraging, but this is the only way to stop the yeast infection from recurring over again.
A yeast infection should never be ignored.
If you have had a past infection, you can easily pass it back and forth to your current partner.
This will not only spread the fungus to them but also to future partners.
If you want to ensure total prevention then you need to learn how is a yeast infection treated.
Learning the answer to the question “How is a yeast infection treated?” Will enable you to learn more ways to prevent the infection from coming back.
There are many home remedies as well as topical creams available in the market.
Also, there are medical procedures where a doctor will remove the excess growths through surgery or by freezing the infection.
How Long Does Vulvovaginitis Typically Last?
The exact answer to this question will vary from one person to the next.
In general, however, many people find that their infections clear up within one week, with a couple of them even having their symptoms disappear.
On the other hand, some people take months or years to completely cure their infections.
As a result, you’ll never know how long you’ll have to suffer from your painful and itchy vulvovaginitis.
Also, the answer to that question of course depends on the type of vulvovaginitis you have.
There are different types of vulvovaginitis including bacterial, fungal, and viral.
And depending on the treatment and the severity of your vulvovaginitis you may have different answers to that question.
As stated before, bacterial vulvovaginitis is one of the easiest to treat.
You may be wondering why that is.
Simple, your doctor is unlikely to prescribe any antibiotics to you for your condition as it is a non-infectious condition.
But, in terms of treating your vulvovaginitis, you may be prescribed a topical treatment such as an anti-fungal cream or gel.
Or, your doctor may prescribe an antibiotic to treat your bacterial vulvovaginitis.
After you have been treated with anti-fungal medication, the next question you may have is, “How long does vulvovaginitis typically last?”.
Also, the answer to this question of course depends on your overall health and how you were exposed to the bacteria or virus that causes your vulvovaginitis.
Some people are more susceptible to certain kinds of vulvovaginitis than others.
And some people’s vulvovaginitis doesn’t recur or show up for several months.
The vulvovaginitis that does reoccur or comes back after a few months may be more severe than the previous infection.
Also, your immune system may not be as strong as it used to be, which can lead to you developing another infection.
Or in the worst-case scenario, allow the previous vulvovaginitis to come back again.
Knowing the answer to this question can help you decide if you should take medication or wait until your immune system improves.
If your vulvovaginitis was caused by an STD, antibiotics may well be required to clear it up.
Your doctor may decide to put you on an anti-fungal medication after taking antibiotics in order to prevent a repeat of your previous infection.
People with STDs almost always use prescriptions in order to clear up their infection.
This is because prescription medications often have stronger chemicals that outlast other anti-fungal treatments.
Anti-fungal medicines are best taken after you have had a course of antibiotics.
The reason for this is that your body will not have time to build up a large amount of a type of toxins.

How Long Does A Yeast Infection Usually Last?
Typically, once you have gotten rid of the source of the infection, you should not have any further problems with it.
You may need to take anti-fungal medication for a little while to make sure that your symptoms are relieved, and then your infection should be gone for good.
However, it is a good idea to seek medical advice if you are having repeated infections.
How long does a yeast infection typically last? You may be able to go away with it, or it may take a few weeks.
If it takes a few weeks, you may want to see a doctor just to make sure that you are getting the right treatment.
And to make sure that there are no underlying conditions causing the yeast infection.
Yeast infections are usually a sign of something that is wrong internally, so to find out what your problem is, you should go see your doctor.
How long does a yeast infection typically last? Normally, they will go away on their own within a few days or even a few weeks.
However, in more extreme cases, they can remain around for a number of months.
If you have never had one before, you should take preventative measures and make sure that you keep the area clean and dry, this will help to keep the fungus from coming back.
Also, if you have had a yeast infection before, then you will probably be able to get rid of it with the right treatment, and the proper information about how to cure it.
The truth is that the answer really lies in your own body.
Yeast infections are usually caused by the overgrowth of certain species of fungus that normally live within and on our bodies.
Candida albicans is the exact name given to this fungus and is considered to be a single-celled fungus.
This does not mean that it cannot be spread, however.
Just because a yeast infection is considered single-celled doesn’t mean that it cannot multiply.
As it multiplies, it becomes much stronger and sooner or later will begin to infect almost every part of the body where it has access to a moist surface.
If the condition gets out of control, there can be serious health consequences.
Most yeast infection sufferers will tell you that the first time they realize that they have an outbreak, it happens very quickly.
There are also some people who have an outbreak multiple times in a short period of time.
In some cases, the fungus can spread from the vaginal area to the mouth, in severe cases it can spread to the esophagus.

What are the symptoms of vulvovaginitis?
Vulvovaginitis is an infection that usually affects women, especially the vulva.
The vulva is the skin around the vagina.
The symptoms of vulvovaginitis may include itching, burning, redness, swelling, and pain.
You may also have a discharge from your vagina.
Sometimes the vulva may appear to be swollen, which is another symptom of vulvovaginitis.
You may also find that there is some bleeding.
However, you should always see a doctor if you are experiencing any of these symptoms.
Do not wait for the condition to worsen.
A doctor can diagnose vulvovaginitis by taking a swab from the vulva.
This will give details about your vulvovaginitis infection.
Other symptoms of vulvovaginitis include a rash in the vaginal area.
Some women feel a lot of pain while having a bowel movement.
Other symptoms of vulvovaginitis include fever, nausea, chills, and general malaise.
You may also feel irritable and tense.
You may experience symptoms like a thin, watery discharge, itching, or burning sensation when urinating.
There are several types of vulvovaginitis, including bacterial and viral.
Vulvovaginitis caused by bacteria is called bacterial vaginosis.
Also, Vulvovaginitis caused by the virus is called candida.
You may also notice an itching sensation in the vagina.
However, don’t mistake this for yeast infection as it can be very dangerous.
If you notice a white curdy discharge along with the symptoms mentioned, you should see a doctor immediately.
He will diagnose the vulvovaginitis infection and help you manage it.
Sometimes, treatment for the symptoms of vulvovaginitis is as simple as just taking a warm bath or applying topical creams.
In some severe cases, the doctor may recommend a course of antibiotics to get rid of the infection.
Usually, the symptoms of vulvovaginitis are not serious and can be treated easily.
Although these symptoms may seem like the result of bad hygiene, it is more likely that you have Vulvovaginitis.
What are the symptoms of vulvovaginitis? The most common symptoms of vulvovaginitis are dryness around the vulva area.
This is a very discomforting condition to deal with.
The symptoms of vulvovaginitis also include painful sex and vaginal odor.
What are the treatments for vulvovaginitis? Treatments for vulvovaginitis depend on the severity of your condition.
If you don’t have severe symptoms, simple over-the-counter medications like hydrogen peroxide and Eucerin will do.
For more severe cases, you may want to consult a doctor.
Common medications for treating vulvovaginitis symptoms include aminosalicylates and azithromycin.
Most women usually take a class of antibiotics to treat their symptoms of vulvovaginitis infection.
See a doctor right away if you start to see symptoms of vulvovaginitis infection.
What are the natural treatments of vulvovaginitis? Some people would prefer to use natural treatments instead of taking antibiotics.
There are actually a lot of things that you can do to treat your symptoms of vulvovaginitis infection.
All you need is some patience and determination in treating your condition.
What are the risk factors for having this condition?
The risk factors of having this disease are pregnancy, STD, diabetes, and sexually transmitted diseases.
If you have one or more of these risk factors, you are more likely to develop vulvovaginitis infection.
The symptoms of vulvovaginitis are actually similar to those of the symptoms of bacterial vaginosis.
You will experience pain while urinating, an unpleasant vaginal discharge, and a fishy odor.
Do not be afraid to seek help from a medical professional, because this condition is not normal.
What Are The Symptoms Of A Yeast Infection?
Anyone can have a yeast infection at any point in their lives.
The symptoms of a yeast infection are not the same for every person, but they usually include a burning, itching, and/or vaginal discharge.
Men can also get these infections, although men rarely get them because their penile pores are smaller than women’s.
Those at greater risk for having a candida infection include:
Babies.
People who frequently wear dentures.
Those taking antibiotics or who have other health issues, including HIV or diabetes.
People who take steroids or who are pregnant may experience symptoms of a yeast infection as well.
These people should seek medical advice to determine if there is an underlying problem that needs attention.
Men.
Men can get candida infections, too.
Common symptoms of a vaginal yeast infection include pain or discomfort during sexual intercourse.
Other symptoms include white discharge from the vagina or itching.
In some cases, men may notice a rash or other abnormal skin changes around the area of the penis.
Women.
Some women will notice that their symptoms don’t clear up right away.
They may develop a yellowish discharge from the vagina, irritation, and burning.
If the symptoms don’t clear up in a few days, they should be seen by a doctor to make sure that it isn’t something more serious.
Female symptoms can include redness, irritation, swelling, pain during sexual intercourse, and/or discharge from the vagina.
Men and women can both develop symptoms of infection when they are sexually active.
When a woman is sexually active, there is a greater chance of transmitting an infection to a man through sexual activity.
Condoms can help prevent men from getting an infection when they have sex.
However, many women do not use condoms and have STDs because they believe that the symptoms of a yeast infection will go away on their own.
Male symptoms of a yeast infection are different than female symptoms of a yeast infection.
If a man has been exposed to antibiotics, he could develop a UTI as well.
This is because antibiotics kill all bacteria in the body, including the good bacteria that are part of the immune system, and keep the bacteria in the urinary tract in check.
There are also symptoms of a yeast infection in babies.
Most of the time, thrush in babies is treated with antifungal medications, which are taken orally once a day.
Rarely, a baby will need to be treated with a prescription medication like an antibiotic because a baby’s immune system is too young to be able to fight off the thrush.
In babies, the treatment may come in the form of special formula or drops that have to be applied to the mouth several times a day.
Some of the other symptoms of a yeast infection include extreme fatigue and dizziness, frequent diarrhea, gas and bloating, irritability, sleep problems, irritable bowel syndrome, respiratory infections, and recurring vaginal infections.
You may also experience a white, thick curd-like discharge and a foul-smelling vaginal odor.
Some women may also develop an itchy rash on their upper thighs.
If you have any of these symptoms, you should contact your gynecologist right away for a proper diagnosis and treatment recommendation.
Thrush can be life-threatening to infants.
It is important to get the right diagnosis and treatment as soon as possible so that your baby’s health can be protected.
Don’t assume that symptoms of vaginal infections are just signs of a general lack of hygiene or a passing phase.
This can be more serious than it seems if left untreated.
Make sure to get medical attention right away if you think that your baby is suffering from any type of vaginal infection.
Some of the other symptoms of a vulvovaginal yeast infection include vaginal discharge that has no odor, a painful itching sensation around the vagina, a change in color (some may be lighter than others), and soreness.
The burning sensation is the most uncomfortable one for a mom-to-be and can make her feel uncomfortable all the time.
Other symptoms of a vulvovaginal yeast infection include a white creamy substance that leaks out of the vagina.
This may come off like cottage cheese when a tampon is inserted and is also quite painful.
Burning can also occur when a man ejaculates, so if you notice this, make sure to have it checked out.
There are many over-the-counter medications that can be used for the symptoms of a yeast infection.
The majority of these medications are topical in nature meaning that they are applied directly to the area that is infected.
They can help to reduce irritation and discomfort, but they are not effective in treating the root cause of this condition.
Women who are pregnant should not use over-the-counter medications because they can make the situation worse, so only treat the symptoms.

Can You Pass Either Condition To A Sexual Partner?
Some people wonder, can vulvovaginitis or a yeast infection pass on to a sexual partner. The answer is yes.
It is quite possible for an infected person to have a partner who is also infected.
In fact, some women may develop an oral yeast infection while they are suffering from a Vulvovaginitis attack.
The reason why some women can have vulvovaginitis or yeast infection while others do not has to do with hygiene.
It is important for women to ensure that any open sores treated with antibiotics are kept dry and are not allowed to get infected with bacteria.
Many women do not practice good personal hygiene and end up spreading the disease to their sexual partners.
This can make it very difficult for the woman to cure her own vulvovaginitis but can allow the infected person to infect a sexual partner.
Other factors that can help explain how can vulvovaginitis or a yeast infection pass on to a sexual partner include a woman’s weight.
Women who are obese tend to develop vulvovaginitis more often than those who are slightly overweight.
Also, women who are pregnant may also find themselves more vulnerable to vulvovaginitis.
Some women tend to develop infections of the vulva more often after giving birth.
This tends to go away on its own but in some cases, the infection can flare up and cause a lot of pain and discomfort during sexual intercourse.
Women who are sexually active with a partner who is infected with a yeast infection have the chance of passing the infection on to their sexual partner.
The main thing to do here is to ensure that the infection is treated so that the symptoms do not get out of control.
This can be done by taking antibiotic medication.
Also, it is important that the infected person is not getting sexually transmitted diseases.
By not having this disease, you will reduce your chances of getting vulvovaginitis or a yeast infection.
Another way of preventing vulvovaginitis from affecting a woman is by using pre-moistened lubricants during sex.
This can prevent friction or any type of rubbing that could bring about an infection.
It will also help in avoiding any type of swelling of the vaginal tissues, which in turn prevents irritation.
Soreness of the vaginal walls can weaken the walls and allow bacterial growth, which in turn increases the chances of vulvovaginitis or a vaginal yeast infection occurs.

Can A Yeast Infection Cause Vulvar Itching?
A yeast infection or Candida Albicans can cause uncomfortable and unpleasant symptoms such as itching, burning, and pain in the vulvar area of the vaginal area.
These symptoms are more common than you think, especially if you have a chronic or recurrent yeast infection.
However, it doesn’t mean that you already have a vulvar itching condition, especially if you have no previous history of candida or irritable bowel syndrome (IBS).
In fact, having the symptoms of an IBS can also mean that you have another condition.
Let’s go back to the question “can a yeast infection cause vulvar itching?”.
A yeast infection is a fungus infection, so to answer that, it would appear that vulvar itching is part of the fungal definition of the ailment.
However, we don’t know this yet, so how do we know which type of yeast infection we have?
In the case of vulvar itching, we know that it is not actually a disease.
While you might have IBS or another similar condition, it will probably be easy to get treated and you won’t need to worry about wondering, can a yeast infection cause vulvar itching?
Now that we have that cleared up, let’s discuss the real causes of vulvar itching.
Some of the most common reasons are topical treatments that are scented or contain perfumes or chemicals.
Although these may make you feel “better”, they can actually cause a reaction that is worse than your current condition.
You should never try to use any type of treatment that makes you think you’re going to feel better – because you’re not.
Another yeast infection cause is clothing that doesn’t fit properly.
Many types of pants or pantyhose don’t sit right on your bottom and this can cause a lot of friction, irritating your skin.
This then creates a good environment for bacteria to grow and the perfect conditions for a yeast infection to set in.
It’s important that you always wear properly fitting clothing and if it doesn’t fit properly, that you exchange it for a new pair.
If you’re still wondering, can a yeast infection cause vulvar itching? The answer is yes.
The problem is that it’s hard to eliminate all of the bacteria from your vagina, even when you change your underwear.
For this reason, many women find that they end up with an additional problem, one that is often much worse than their current vulvar itching.
Conclusion.
One of the most important things that you should be aware of when you decide to read up on vulvovaginitis or yeast infection is the role that diet plays in the development of this condition.
A good diet can help to improve your overall health and well-being which is why it is a very important topic.
If you happen to have a poor diet and are suffering from vulvovaginitis then the best way to treat the condition is to follow a diet for pre-menopausal women that are low in sugar and high in complex carbohydrates.
Complex carbohydrates like pasta and foods that are high in sugar aren’t good for you and should be avoided altogether.
Another thing that you should be aware of when you read about vulvovaginitis or yeast infection is the role that clothing plays.
For instance, it has been found that certain types of clothing actually can contribute to the development of this condition.
Also, it is important to make sure that you are wearing the right type of underwear.
The purpose of underwear is to keep your genitals clean and dry at all times.
Therefore, if you happen to wear a type of underwear that allows moisture to build up around the genital area then you may find that this can actually worsen your vulvovaginitis rather than help you.