The warning signs of vulvar cancer are often the same as for breast or prostate cancer.
The main difference is in the stage.
Stage IVB can be any size and can spread to nearby lymph nodes and distant organs.
It is extremely important to be tested for vulvar cancer early to prevent it from progressing to the more advanced stages.
The good news is that treatment options for vulvar cancer are widely available.
Table of Contents
What Are The Warning Signs Of Vulvar Cancer – Ultimate Guide
Symptoms
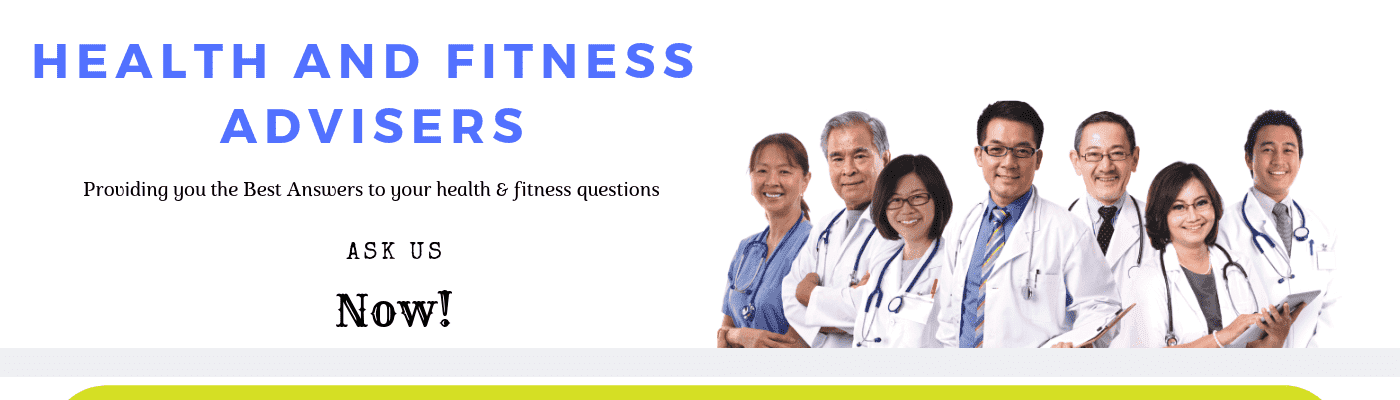
Vulvar cancer affects the vulva, the outermost part of a woman’s vagina.
It can originate in the clitoris or the labia majora, and it may spread to other parts of the body.
Also, it can cause serious pain and unusual bleeding.
Early symptoms of vulvar cancer include bleeding and itchiness.
Also, early detection is possible with regular smear tests.
Changes in the color of the vaginal lips can also help detect the early stages of vulvar cancer.
Vulva includes the labia majora, mons pubis, clitoris, and the lesser and greater vestibule.
In the early stages, cancer may not spread beyond the vulva.
The first few lymph nodes near the cancerous area are removed.
This test will determine if the cancer has spread.
If no cancer is found, additional lymph nodes may not be necessary.
Cancer may spread to the bowel, anus, or perineum.
When it spreads to lymph nodes, it is considered stage III.
If these symptoms are present, your healthcare provider may recommend further tests to determine the type of cancer and whether it has spread.
Additional tests may include a blood test, chest x-ray, proctoscopy, or a computerized tomography scan.
If the diagnosis is made, you may experience feelings of disbelief, shock, and anxiety.
Ultimately, you must take action and seek medical attention immediately.
Other symptoms of vulvar cancer include unusual lumps, ulcers, or bleeding in the vulva.
In addition to pain during intercourse, you may also experience itching, burning, or discharge.
The pain may be mild, or it may be an indication of another condition.
During the course of your treatment, your healthcare provider will ask you to answer questions about your lifestyle, medical history, and other conditions you may have.
Imaging scans may also be necessary to confirm the diagnosis.
Treatment options for vulvar cancer depend on the type and stage of your cancer.
The goal of treatment will depend on the type and stage of cancer, whether you wish to have a future pregnancy, and the level of cancer you have.
Treatment options may involve surgery or other treatments to control or ease your symptoms.
Your healthcare team will discuss the options available to you and your loved ones.
However, you should be sure to ask your healthcare team about the risks and benefits of your chosen treatment.

Treatment options
Treatment for vulvar cancer depends on the type and stage of the disease, as well as the patient’s preferences and overall health.
There are two main types of surgery: radical vulvectomy and partial vulvectomy.
Radical vulvectomy involves removing the entire vulva, along with its lining and lymph nodes on both sides.
Partial vulvectomy involves removing part of the vulva.
Skin vulvectomy is a surgical procedure that removes the top layer of the vulva, sometimes requiring skin grafts.
The modified radical vulvectomy removes part of the vulva and some healthy tissue surrounding cancer.
Radical vulvectomy removes the entire vulva, including the clitoris, cervix, and lower colon.
Depending on the location of the cancer, it may be necessary to remove the entire vulva.
If your vulvar cancer is advanced, your doctor may recommend chemotherapy.
This treatment may be combined with radiation therapy to shrink the tumor and improve the chances of surgery.
If the cancer is not terminal, treatment can be repeated as needed to reduce the risk of side effects.
Your physician may recommend regular follow-up exams to monitor cancer and make sure that no treatment options are unnecessary.
This way, you’ll know whether the cancer has spread and how long it will take to get better.
Early detection is the key to a successful outcome.
Also, early diagnosis is key to vulvar cancer treatment.
Even if it has spread, vulvar cancer is highly treatable if detected in its earliest stages.
However, precancerous cells can grow on the vulvar skin for years before it turns into cancer.
As they continue to accumulate, they form a tumor and invade surrounding tissue.
Cancer may also spread to other parts of the body.

Risk Factors For Vulvar Cancer
There are a number of risk factors for vulvar cancer, including HPV infection, cigarette smoking, and STIs.
Although experts don’t know why cells grow too quickly, there are certain factors that increase the likelihood of developing vulval cancer.
Treatment for this type of cancer depends on its stage.
If you have vulvar cancer or have it on a family member, you should seek treatment immediately.
HPV infection increases the risk of vulvar cancer
Vulvar cancer is caused by abnormal cells that grow at an uncontrolled rate.
This precancerous condition is called vulvar intraepithelial neoplasia (VIN) and is commonly associated with HPV infection.
Women who develop VIN have a significantly increased risk of developing invasive vulvar cancer in the future.
The good news is that the disease is treatable.
There are several things you can do to reduce your risk.
The authors noted that there is considerable geographic variation in the percentage of vulvar cancers that are HPV-positive.
This may be related to the low number of specimens analyzed for this study.
Further studies are needed to confirm the association between HPV infection and vulvar cancer risk.
Cigarette smoking increases the risk of vulvar cancer
Women should be aware that cigarette smoking increases their risk of vulvar cancer.
Cancer begins when cells have DNA mutations.
DNA is the instructions for cells, and when these mutations occur, cells begin to multiply quickly and divide abnormally.
These abnormal cells can survive when normal ones would die.
As a result, a tumor forms.
This tumor can invade nearby tissues and can spread to other parts of the body.
Vulvar squamous cell carcinoma begins in thin, flat cells.
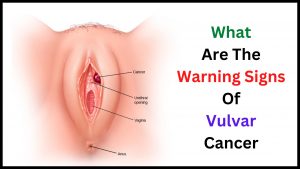
Melanoma is usually a pigment-producing tumor.
Studies have shown that cigarette smoking increases the risk of vulvar cancer by a factor of five.
The risk of vulvar cancer was highest in women who smoked for at least five years.
Researchers also found a strong association between smoking and certain genital infections in women who smoke.
Cigarette smoking is also associated with higher rates of Chlamydia trachomatis, Trichomonas vaginalis, and herpes simplex virus type 2.
In addition, research has linked cigarette smoking to cervical pre-cancer and damage to the cervical epithelium.
STIs are a risk factor for Vulvar Cancer
There are several known risk factors for vulvar cancer, including STIs, weakened immune systems, and aging.
However, there is no definitive cause.
The vulva is most often affected by older women, with only about 20% of new cases occurring in women younger than 50.
However, there have been some cases of young women developing the disease as well.
In such cases, there is a high likelihood that the condition is caused by an STI.
Although vulvar cancer is a rare disease, it is treatable when caught early.
There are several ways to detect the disease, including ultrasound and CT scans.
In addition to ultrasound, MRI can be used to identify vulvar cancer.
MRI scans can show high signal intensity in the vulva, which indicates the presence of a tumor.
Patients can receive radiation therapy or chemotherapy, as needed.

Treatment Options For Vulvar Cancer
Treatment options for vulvar cancer depend on the stage, grade, and general health of the patient.
Surgery may include local excision of cancer, as well as the removal of the cervix, bladder, and lower colon.
In some cases, cancer may spread and require a vulvectomy to remove it completely.
Chemotherapy may also be used to destroy cancer cells while reducing the size of the tumor.
However, this option is not appropriate for all patients.
Radiation therapy and chemotherapy are two options for treating vulvar cancer.
Both of these options use high-energy rays to kill cancer cells.
Radiation therapy, on the other hand, is a local therapy, meaning it is only applied to the vulva.
And radiation therapy is usually performed in combination with chemotherapy.
It is used when surgery is not enough to completely remove cancer.
and it can also be combined with other forms of treatment.
In addition to radiotherapy, doctors may also perform tests to detect whether cancer has spread to distant parts of the body.
A chest x-ray will detect if it has spread to the lungs or lymph nodes.
Also, a computed tomography (CT) scan is another diagnostic test used to detect vulvar cancer.
MRIs are useful for identifying tumors inside the pelvic area and identifying enlarged lymph nodes in the groin.
MRIs may not be necessary if the vulvar cancer is caught early.
Other tests used to assess cancer spread to distant areas of the body include positron emission tomography (PET), which generates three-dimensional images of the human body.
Surgical treatments for vulvar cancer depend on the stage of the disease.
In some cases, the entire vulva or a portion of it is removed.
In others, the vulva and the underlying tissues are removed.
A radical vulvectomy, on the other hand, requires the removal of the entire vulva and all surrounding tissue.
Some women have to undergo multiple surgeries before they receive successful treatment.

Vulvar Cancer Signs to Watch Out For.
There are several vulvar cancer signs to look out for, including general changes in your body.
Although these changes are only known to you, other people may notice them.
The signs can be indicative of a different medical problem than vulvar cancer.
For example, you might not be experiencing any of these symptoms, even if you have no symptoms.
But if you notice them, you should see your doctor immediately.
General Signs Of Vulvar Cancer
Although vulvar cancer is rare, it can occur.
The most common signs to watch out for are irregular bowel movements and problems passing urine.
There are also secondary cancers that can cause weight loss, aching bones, and fatigue.
Some skin conditions can also be indicative of vulvar cancer, such as lichen sclerosus.
Vulval intraepithelial neoplasia, or VIN, is also a type of pre-cancerous growth that has a high risk of becoming cancerous if left untreated.
In women, the chances of developing vulvar cancer are five to 10 percent.
And in contrast, women with basal carcinoma are at a much lower risk of developing vulvar cancer.
Despite the fact that vulvar cancer is rare, women who are HIV-infected or have poor immune systems are at a higher risk for it.
Those with weakened immune systems have an increased risk of developing the disease, so preventing this infection is especially important.
While there is no single test for vulvar cancer, women who are at increased risk should be evaluated by a doctor for a pelvic exam to determine whether they have any of these conditions.
Symptoms Of Vulvar Cancer Type
Symptoms of vulvar cancer type vary between types.
While vulvar cancer commonly affects women after menopause, it can affect women of any age.
In Australia, there are an estimated 433 new cases of vulvar cancer each year.
It is difficult to self-examine the vulva, but you should see a doctor if you notice any changes.
While the disease is relatively rare, symptoms may include pain in the genital region, hardness in the groin area, or unusual bleeding.
Treatment for vulvar cancer may include surgery and radiation therapy.
Radiation therapy can kill cancer cells without causing any damage to the surrounding tissue.
Chemotherapy is another treatment option.
It can help control secondary cancers while restoring a woman’s quality of life.
Patients may also receive oral medications or injectable drugs.
While treatment for vulvar cancer varies, it can be managed and controlled with a healthy lifestyle and regular checkups.
Some women who develop vulvar cancer may also experience a variety of other symptoms.
Also, some women experience bowel symptoms such as difficulty passing urine and a feeling of displeasure.
Other symptoms of vulval cancer include loss of appetite, fatigue, and aching bones.
The vulva is also a common site for skin conditions such as lichen sclerosus.
Precancerous lesions, such as vulval intraepithelial neoplasia (VIN), have a higher risk of developing cancer if left untreated.
The prevalence of vulval cancer is comparatively low – about five to 10 percent of women develop it.
Basal carcinoma is the most common type and is caused by long-term exposure to HPV.

Vulvar Intraepithelial Neoplasia
Vulvar intraepithelial nevus, or VIN, is a precancerous growth of cells that develop in the vulva.
It is treated differently from invasive Vulvar cancer.
These lesions are classified according to the type of cells and can be classified into two groups: squamous and keratinizing.
In some women, VIN may develop after having an ongoing infection with HPV.
A biopsy is one way to diagnose Vulvar cancer.
Also a small sample of skin from the vulva is removed.
It’s generally done after a local anesthetic has numbed the skin.
A sample of cells is analyzed to determine if they are typical VIN cells.
Treatments may involve the removal or destruction of all affected tissue.
Your doctor will discuss the risks and benefits of each method.
If you notice melanoma on your vulva, it’s time to seek medical attention immediately.
Melanoma is rare in the vulva.
However, squamous cell cancer is the most common form of the disease.
The vulva is made up of two main areas: the clitoris and the labia majora.
In most cases, the cancer is asymptomatic, and if it’s detected early enough, it can be treated.
Invasive Squamous Cell Cancer Of The Vulva
There are many vulvar cancer signs to watch for.
A small number of these are sarcomas, which are tumors that begin in tissue and grow quickly.
Different types of sarcomas form in different tissues.
Leiomyosarcomas develop in muscle tissue, while angiosarcomas develop in blood vessel cells.
Both types of cancers affect the vulva’s surface, similar to breast and skin cancer.
Stage IA is the earliest stage of cancer and occurs in the vulva and perineum.
Cancer has grown into nearby tissue but has not spread to distant tissues or lymph nodes.
Stage II or III cancer may also affect lymph nodes in the groin or distant parts of the body.
Your doctor may remove sentinel lymph nodes in the vulva to check for the spread of cancer cells.
And your doctor may also remove these lymph nodes depending on the size of your tumor.
If the cancer is detected early, doctors may remove the sentinel lymph nodes to help with staging the disease.
Also, if there’s no evidence of cancer spread, doctors may recommend a biopsy of the sentinel lymph nodes to find out if cancer cells have spread to nearby tissues.
Vulvar Melanoma
There are some vulvar melanoma signs to watch for.
Itchy, crusty, or bleeding vulva may indicate a serious underlying problem.
Bleeding and itching may also indicate thrush.
If you notice any of these symptoms, you should see your healthcare provider as soon as possible.
In many cases, you may be experiencing only one of these symptoms.
Your doctor may recommend palliative treatment to improve your quality of life and slow the progression of the disease.
This form of treatment is best thought of as supportive care.
Palliative care may be beneficial at any stage of the disease, even if it is advanced.
These treatments can improve your symptoms while slowing down tumor growth.
You should discuss your treatment options with your health care team so that you can make an informed decision.
If cancer has spread to nearby lymph nodes, treatment will depend on the stage.
Stage III refers to cancer that has spread to nearby lymph nodes.
And stage III is most appropriate for newly diagnosed cancer that has spread to nearby lymph nodes.
Treatment options will depend on the type of vulvar melanoma and other factors.
If cancer has spread throughout the vulva, surgery may be the best option.
Patients who have undergone this type of surgery may require additional testing and treatment.
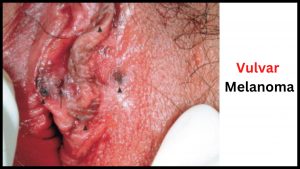
Bartholin Gland Cancer
A diagnosis of Bartholin gland cancer should be made in patients who exhibit atypical characteristics.
It may arise in the gland or duct.
ACCBG is composed of small cells arranged in cords or nests.
Associated with atypical characteristics are acellular spaces with variable mucin and hyalinized materials.
Surgical removal is the standard treatment for Bartholin gland cancer.
The most common sign of Bartholin gland cancer is a distinct mass near the opening of the vagina.
And the mass is more likely a benign cyst than a cancerous mass.
Other symptoms include soreness and redness in the vaginal region, and pain while urinating.
The mass may also be sore or scaly.
While the most common symptom of Bartholin gland cancer is a lump in the vagina, it can be a sign of another complication, such as Paget’s disease of the vulva.
In stage II and stage III, cancer cells have spread to nearby tissues or lymph nodes, which means that the tumor has spread.
Stage IV cancer has spread to distant areas of the body.
Surgery may include the removal of the entire vulva or part of it.
The doctor may also perform pelvic exenteration, which removes the lower colon, rectum, and cervix, as well as affected tissue.
Radiation therapy may also be necessary.

Paget’s Disease Of The Vulva
The signs and symptoms of Paget’s disease of the vulva are similar to those of other vulvar rashes.
During the initial diagnosis, a biopsy will confirm the condition, but some patients are asymptomatic at the time of the diagnosis.
In some cases, a doctor may recommend a cystoscopy or a colonoscopy to rule out bladder or colon cancer.
However, bladder or colon cancer is not common with this condition.
Invasive Paget’s disease of the vulva is characterized by a large, red mass in the vulva that is larger than four centimeters in size.
This mass can be macroscopically observed as a 4.3×3.6 cm vulvar tumor.
On examination, the patient had an erythematous rash throughout the vulva.
Also, on a computed tomography (CT) scan, the affected area had enlarged lymph nodes on the left side of the obturator.
A frozen section was also used to evaluate the margin.
The first sign of Paget’s disease of the vulva is the appearance of red and white patches of tissue or scaly skin.
The condition may also be pink or moist and may be accompanied by itching.
Women who suffer from the disease are often postmenopausal.
Surgery for the disease is typically recommended.
Skin grafting is sometimes necessary.
Treatment Options
When a woman is experiencing vulvar cancer symptoms, it’s important to know what to look for.
During an exam, your doctor will check your vulva for lumps, sores, or unusual signs.
Further tests, such as a PET scan, will be done to determine whether the cancer has spread.
Your healthcare provider will explain the stage of your disease to you before deciding on a course of treatment.
Chemotherapy is a treatment that uses medications to kill cancer cells.
The drugs are usually administered intravenously but may be given as pills, creams, or injections in the vulva.
And the treatment cycle involves several treatments, separated by rest periods.
In some cases, the treatment can be done as an outpatient, while others may need to stay overnight in the hospital.
This can cause sexual problems or decreased libido.

How Do I Check Myself For Vulvar Cancer?
To check yourself for vulvar cancer, you may feel that you have noticed a lump or ulcer on your vagina.
These symptoms may be harmless or they may indicate a more serious condition.
A doctor will perform a biopsy on the tissue you notice.
Also, a pathologist will analyze it under a microscope to determine whether it is cancerous.
The test can be done with or without general anesthesia, depending on the type of vulvar cancer you have.
Before you start your self-examination, you must have a mirror.
To properly check yourself, you should examine the pubic area, clitoris, vaginal opening, and labia majora/minora.
Also, feel for any lumps or bumps under the surface.
The area around your vulva may become sore, swollen, or pink.
It may also bleed.
In addition, you may feel a burning sensation or a strange smell.
During this period, your treatment team will give you creams to reduce the pain and speed up your recovery.
And during this time, you should avoid heavy lifting and driving, but don’t worry if your pubic hair is falling out.
Hair growth is not a result of cancer.
You may also need to consult a medical professional for a proper diagnosis.
If you have any concerns or suspect vulvar cancer, you should get a thorough examination from a doctor or qualified health professional.
The results of vulvar cancer tests will tell your doctor whether your cancer has spread or is still small.
If the cancer is small and has not spread to other parts of the body, it is still treatable.
The doctor will assess the condition and the stage of the disease to determine the best course of treatment.
During the process, your doctor will take into account the results of your tests, your age, and your overall health.
Your doctor will also discuss your treatment options and your prognosis.
Many women fail to look at their vaginas.
It is difficult to examine the vagina without a mirror, and some women are embarrassed to do so.
However, even the slightest change could indicate a precancerous condition.
In some cases, VIN can be benign, but most women require treatment to prevent the condition from progressing to cancer.
The symptoms of vulvar cancer will be vague, and your doctor will need to perform tests to rule out other conditions.
Surgical treatment depends on the stage of the disease.
Advanced vulvar cancer may require a surgery called pelvic exenteration, which involves removing the entire vulva and a part of the bowel.
Although it is a major operation, it is not performed very often.
A diverted bowel, which involves making an incision in your tummy, will divert your bowel to another part of your body.
Treatment may include chemotherapy, a type of treatment that aims to slow the growth of cancer cells.
The drugs are usually administered by mouth, but they can also be applied to your vulva with a lotion or cream.
The type of chemotherapy given will depend on the stage and type of cancer.
Once the vulvar cancer is detected, the doctor will recommend an appropriate treatment.
In the meantime, you may experience some symptoms that may be symptomatic.
Prognosis
A doctor’s assessment of your prognosis for vulvar cancer will depend on the location and extent of cancer.
In most cases, the cancer is locally limited and cannot spread to other parts of the body.
However, if cancer has spread, the prognosis may be more uncertain.
A doctor will explain your options and timelines, and discuss side effects and possible risks of various treatment options.
The prognosis of vulvar cancer is different for patients with a prior history of radiation treatment.
The gold standard of treatment for vulvar cancer is surgical resection.
A tumor with a 1 cm margin is usually excised during a vulvectomy.
However, if cancer has spread to nearby organs, it may require a radical vulvectomy.
Surgical removal of the tumor is crucial for identifying the extent of the disease and deciding on the course of treatment.
The risk of amputation is higher in vulvar cancer, however than in most other types.

Which Symptom Is An Early Symptom Of Vulvar Cancer?
The earliest warning signs for vulvar cancer include any of the following:
Stage I vulvar cancer is typically confined to the vulva and perineum.
However, it can also spread to the anus, lower third of the vagina, and the urethra.
Cancer cells have spread to other nearby organs or lymph nodes.
It can be spread to other parts of the pelvic cavity, but it has not yet spread to distant organs.
Therefore, stage IB cancer is typically considered in the early stages.
The main early warning signs of vulvar cancer include bleeding, discoloration, pain, and lumps in the vulva.
And the last symptom, vulvar discoloration, is also common.
If a lump is present, it could be cancer spreading to the rest of the body.
Although vulvar cancer may occur in a woman with vaginal sclerosus, most survivors survive for at least five years after diagnosis.
The most common form of vulvar cancer is caused by human papillomavirus (HPV) subtypes.
Other risk factors for the development of vulvar cancer include advancing age, family history of melanoma, HIV, and lichen sclerosis.
Smoking and other genital cancers are also associated with an increased risk of developing the disease.
Early symptoms may be non-existent, but doctors can detect vulvar cancer by its presence in the vagina.
Surgical treatment may be necessary.
Treatment options vary depending on the stage of cancer and how it has spread.
Another common type of vulvar cancer is squamous cell carcinoma, which begins in thin flat cells in the lining of the vulva.
Most vulvar cancers grow slowly and are relatively harmless, but a few can spread very quickly and invade the pelvis, urethra, or anus.
If left untreated, vulvar cancer can eventually spread to lymph nodes or the bloodstream.
Other symptoms may be the same as those from other causes.
Some women may not know they have vulvar cancer until it has spread to the perineum.
While some women have no symptoms at all, others may experience problems passing urine and bowel motions.
If these signs persist, it’s best to schedule an appointment with your primary care physician or gynecologist.
You can also sign up for a free health newsletter to stay up-to-date on current health topics and diseases.
The vulva is a very common site of skin cancer, including lichen sclerosus and vulval intraepithelial neoplasia (VIN).
The risk of VIN becoming cancerous is very high if not treated.
It’s estimated that only five to 10 percent of women develop vulvar cancer.
Several other rare forms of skin cancer are known to be more common, including basal carcinoma.
The doctor will perform a vulvar exam during which he or she will look for any signs of cancer.
And the physician will examine the perineal region, as well as the urethra and clitoris, to look for abnormalities.
A biopsy of tissue will be taken and analyzed for signs of cancer.
Depending on the type of vulvar cancer, the tumor may spread to other parts of the body, such as the lungs.
During chemotherapy, drugs are given to prevent the cancer cells from growing and dividing.
The drugs are commonly given intravenously or in the form of a cream that is applied directly to the vulva.
Most women receive several sessions of chemotherapy and a rest period between them, which is known as a cycle.
Treatment may be done as an outpatient procedure or as an inpatient stay in the hospital.
Patients may also require a follow-up visit.

How Quickly Does Vulvar Cancer Develop?
Usually, vulvar cancer develops over a long period of time.
It begins as precancerous cells, which may then grow and turn into cancer.
You should be aware of the symptoms, including pain and swelling.
If left untreated, vulvar cancer may spread throughout the body.
Regular examinations may help detect these cells early, which can lead to early treatment.
Once detected, vulvar cancer can be treated if you notice any abnormal changes.
If you notice any of these symptoms, see your doctor immediately.
The stage of cancer is important because it allows doctors to decide if more treatment is necessary.
It also lets them assess your prognosis.
The stage of the cancer is based on the size, location, and spread of the disease.
FIGO, the International Federation of Obstetrics and Gynecology, developed different stages.
Your doctor will use these stages to assess the size of cancer and whether it has spread to other parts of the body.
If the tumor grows more than 2 centimeters and has reached the perineum, then it is considered stage IB.
It may also spread to nearby lymph nodes or the anus.
Stage II tumors have spread beyond the vulva and perineum and may have invaded nearby organs.
The final stage is called stage IV.
It has spread to lymph nodes and distant organs.
Most vulval cancers develop from a gland on the vulva’s surface.
These cancers are called adenocarcinomas.
Other types of vulvar cancer develop from glands in the vulva, such as the Bartholin’s gland.
These glands produce mucous and make lubrication during sexual intercourse.
Bartholin’s gland cancer is rare and is not very common.
The second type of vulvar cancer develops from cells in the deepest layer of the vulva.
Basal cell carcinomas grow slowly and look like large warts.
When a woman has suspected cancer, a physician may take a small sample of the suspicious area and send it to a laboratory for examination.
The pathologist will then look at the cells under a microscope to determine whether it is cancer or not.
It is important to note that a Pap test cannot diagnose vulvar cancer, so you should always have it done by a doctor.
If the tumor is detected early, the symptoms can be treated.
A lump, itching, bleeding, discoloration of the skin, pain, and discoloration of the vagina may be symptoms of vulvar cancer.
If left untreated, vulvar cancer may spread to other parts of the body.
To detect early stages, you should have regular smear tests.
In addition, you should check your vaginal lips for any changes.
Your doctor may recommend treatment with radiation therapy if the cancer is detected early.

Does Vulvar Cancer Make You Feel Sick?
Some symptoms of vulvar cancer include abnormal vaginal bleeding, pelvic pain, and ulceration.
Bleeding can be heavy, irregular, or long-lasting.
It may also be associated with constipation.
Some women also report pelvic pain during urination or during sex.
If you experience any of these symptoms, you should consult a doctor.
The first step in treating vulvar cancer is addressing your symptoms.
A health newsletter can help you manage your symptoms and learn about current topics.
Sign up for an online newsletter to stay informed about health topics.
Treatment may include reconstructive surgery.
Your surgeon may suggest skin flaps or grafts reconstruct your vulva.
More aggressive treatment may involve immunotherapy.
These treatments use natural or synthetic substances to fight cancer.
Follow-up visits are necessary to check for the progress of your cancer and to determine if your symptoms have improved or become worse.
Even after the surgery, you should go for follow-up visits and be aware of any changes in your body.
The emotional impact of vulvar cancer is significant.
Many people report a roller-coaster effect when undergoing treatment for vulvar cancer.
They feel low after diagnosis, then high after surgery.
Some suffer from depression following surgery or treatment.
If you notice any of these symptoms, consult your doctor immediately.
There are various treatment options available for depression and you can ask for more details.
You can also ask for a self-examination if you are unsure if you have the disease.
When the cancer is advanced, the only treatment options are exenteration or a hysterectomy.
Pelvic exenteration involves removing part of the vulva, the womb, and a portion of the bowel.
This method also removes the lymph nodes in the pelvic area.
However, pelvic exenteration is an option for women with advanced vulvar cancer.
A sentinel lymph node biopsy is another treatment option for women with vulvar cancer.
The first lymph nodes surrounding the tumor are removed and tested to find if it has spread to other areas.
If no cancer is detected, additional lymph nodes may not be needed.
Also, if cancer has spread to the lymph nodes, a sentinel lymph node biopsy is also recommended.
It will show the extent of the disease and the likelihood that cancer will spread to other organs.
Early detection is critical to the survival rate of vulvar cancer.
Also, early diagnosis and biopsy are the keys to curing vulvar cancer.
Follow-up appointments are vitally important, especially after surgery.
During this time, you may notice some changes in your body, which you should discuss with your healthcare provider.
If you’re concerned about your appearance, you should let a friend or family member know so that they can provide support during your difficult time.
Is Vulvar Cancer Curable?
As with any disease, early diagnosis improves the outlook for the patient.
Although there are many ways to tell if you have vulvar cancer, the most common symptoms include bleeding, ulceration, and a lump.
You should see your doctor if any of these symptoms persist for more than a week.
Symptoms of vulvar cancer can differ based on the type and stage of the disease.
Regardless of age or gender, you should visit a physician if you notice any of these symptoms.
Early detection is the key to a woman’s long-term health.
According to the National Cancer Institute, the relative five-year survival rate of patients with vulvar cancer is 71 percent.
This percentage is higher if the disease is diagnosed early, as only 40 percent of those who develop stage four cancer survive that long.
Detection and treatment of VIN are essential to a woman’s long-term health.
While the Office of National Statistics does not provide vulvar cancer survival statistics, there are still positive signs to look out for.
If you suspect vulvar cancer, your doctor may recommend a sentinel lymph node biopsy.
This procedure involves removing the first few lymph nodes that surround cancer.
And this way, doctors can determine whether or not cancer has spread to the lymph nodes and if there are any other lymph nodes in the pelvis.
Surgical removal of these nodes reduces the risk of cancer recurring.
Your doctor may conduct several tests to diagnose the disease.
A proctoscope, an instrument used to look inside the rectum and anus, is used to examine the vulva and determine if the disease has spread.
The results of the scan can also help determine what treatment is most appropriate for you.
You may also undergo imaging scans to monitor your cancer’s progress.
The doctor may use an MRI, CT scan, or TC scan to determine how far the disease has spread.
Treatment for vulvar cancer depends on the type and stage of the disease, as well as the patient’s preferences.
The team may recommend a combination of medications or may prescribe chemotherapy or other treatments to slow its growth.
Also, the aim of these treatments is to improve your quality of life and minimize any side effects that may result from the treatment.
In addition to improving quality of life, palliative care may be beneficial, regardless of the stage of your disease.
While the treatment options for vulvar cancer depend on the type of cancer, many women do not have to undergo surgery in order to manage their symptoms.
A surgeon may recommend surgery to remove the disease and test for nearby cancer.
During surgery, a surgeon may also use laser surgery or medication to target the abnormal areas.
If the VIN is extensive, the doctor may recommend partial surgical removal.
The surgery does not remove the fatty tissue beneath the skin.
And the surgery may include topical therapy.
The treatment for stage II vulvar cancer varies, depending on its location and size.
When cancer is at this stage, it has spread to nearby organs, such as the vagina and the anus.
It can also spread to nearby lymph nodes.
Also, it is best to undergo surgery in stage II if the tumor is small and does not spread to nearby organs.
Afterward, the healthcare provider may recommend radiation therapy or chemotherapy.
Treatment for vulvar cancer depends on the stage of the disease, the type of disease, the stage, and your overall health.
Treatment options for this disease may involve surgery, radiation therapy, or chemotherapy.
Many women combine all three treatments, depending on the type and location of cancer.
Surgical treatment for stage one vulvar cancer is most effective in preserving sexual function, but some women may need regular checkups after treatment to monitor its progress.
Chemotherapy focuses on using the body’s own immune system to fight cancer.
It may be administered via injections or as a cream.
It can be given as an intravenous or topical treatment, and it is usually administered during several treatment sessions.
Treatment sessions may include several resting periods between treatments, known as a “cycle.”
External beam radiation therapy can be effective for metastatic vulvar cancer.
This type of treatment does not require anesthesia and is painless.
However, it does have a risk of causing radiation-induced side effects, and its long-term effect may require a different type of treatment.
In addition, if your cancer has spread beyond your ovary, you will need surgery.
However, if you have good overall health and are undergoing treatment, vulvar cancer is usually curable.
Conclusion:
If you have any of the warning signs of vulvar cancer, you should contact a doctor to get a proper diagnosis.
Early detection is crucial for the best outcome.
If you notice a lump, ulceration, itching, irritation, bleeding, or changes in the area around the vulva, you should visit a doctor for a proper diagnosis.
Cancer is a disease that occurs when the growth of cells in the body is out of control.
There are a variety of treatment options for vulvar cancer.
A biopsy may be needed to determine whether the condition is curable.
Also, biopsy involves taking samples of tissue from the vulva.
This procedure may involve a local anesthetic to minimize pain.
Once the biopsy is performed, a gynecologic oncologist (a specialist in cancer of the female reproductive system) will review the findings.
If they detect a cancerous tumor, the doctor may order more tests.
The first warning sign of vulvar cancer is pain during sex.
This pain may affect a woman’s ability to achieve orgasm or pee.
After undergoing surgery, reconstructive surgery may be needed.
Other treatments include biological therapy, which involves the use of natural or synthetic substances to treat cancer.
It is important to attend follow-up visits and be vigilant of changes in the area around the vulva.
Surgical treatment is the most common form of treatment for vulvar cancer.
The type of surgery used will depend on the stage of the disease and the overall health of the patient.
For early-stage cancer, a surgeon may perform a local excision that removes only cancer and the normal tissue surrounding it.
For later stages, a surgeon may perform a full-blown vulvectomy.
A partial vulvectomy, on the other hand, may involve a smaller surgery.