The cancer of the vulvar typically grows slowly over several years.
This is because precancerous cells begin to grow on the vulva’s surface.
These precancerous cells are called vulvar intraepithelial neoplasia or dysplasia.
If the tumor is located deeper than the epithelial junction of the most superficial adjacent dermal papilla, then cancer has advanced to stage 1.
If you have noticed these symptoms, you may have stage 1 vulvar cancer.
Table of Contents
Stage 1 Vulvar Cancer Symptoms: Causes, Diagnosis & Treatment
This type of cancer does not spread outside of the vulva.
It is classified according to the size of the tumor and the location in the vagina.
Cancer has not spread more than 1 mm into surrounding tissue, and there are no signs of distant disease.
While stage 1 vulvar cancer may not spread beyond the vulva and perineum, it can spread to the anus and lower thirds of the vagina.
Cancer cells may also spread to the lymph nodes in the pelvic region.
It is important to see a doctor as soon as possible.
During a vulvar cancer diagnosis, your physician will perform several tests to determine the tumor’s size and location.
They may also order imaging scans, such as a TC scan or an MRI.
These tests can classify cancer and determine the appropriate treatment plan.
The earliest possible treatment for stage 1 vulvar cancer is surgery.
Your doctor will likely order a biopsy to confirm the diagnosis.
Symptoms of vulvar cancer may include pain, ulceration, itching, irritation, or bleeding in the vulva.
It may be difficult to see these changes without a mirror and can be very uncomfortable for some women.
However, you should consult your doctor if you notice any of these symptoms.
While early detection can prevent the spread of the disease, you should never delay a visit to your doctor.
A doctor will perform a physical examination and will also ask about your lifestyle.
Once the diagnosis of stage 1 vulvar cancer is confirmed, treatment options depend on the stage of cancer and how far it has spread.
Treatment options for stage one vulvar cancer may involve surgery and chemotherapy.
Depending on the location and extent of cancer, surgery will remove the tumor from the vulva while preserving as much healthy tissue as possible.
Surgery may also include laser surgery.
A surgeon will cut out cancer with a thin margin or a deeper margin.
The surgeon may also perform lymph node dissection in order to ensure that there are no abnormal lymph nodes around cancer.
Surgery for stage one vulvar cancer will include a biopsy of the affected area.
The cancer is large enough to spread to nearby lymph nodes and organs.
It is best to seek medical attention if you suspect that cancer has spread.
After the surgery, the doctor may recommend reconstructive procedures such as skin flaps and grafts.
There are also immunotherapies, which use natural or synthetic substances to treat cancer.
After the cancer has been removed, a follow-up visit will be needed to monitor cancer’s progress.
Another symptom of vulvar cancer is a sore or bleeding knot.
In addition to these, the vulva may also have a patch of skin, called the perineum.
However, these patches of skin may be caused by other conditions.
One of the most common types is squamous cell carcinoma, which starts in skin cells and may be related to the human papillomavirus.
Another type is verrucous carcinoma, which looks like a wart.
Symptoms of vulvar cancer are similar to those of ovarian cancer.
Generally, cancer develops slowly over several years, and its symptoms begin to appear when the patient is over age 65.
However, women between 40 and 75 years of age can also be affected.
HPV infection and smoking are risk factors for developing vulvar cancer.
Treatment for vulvar cancer involves surgery.
The survival rate for vulvar cancer is around 70%.
During treatment, the vulva may become sore, pink, or red.
And it can be itchy and blistered, or it may even weep.
It is essential for women to rest and dry the vulva area carefully.
After surgery, the patient will be advised to avoid wearing tight clothes for six to eight weeks.
During this time, it is also important to follow instructions given by the treatment team.
Sexual intercourse should be delayed until the vulva has recovered.
While treatment for vulvar cancer may not cure cancer, it can greatly improve the quality of life for patients.
The aim of palliative care is to provide comfort and relieve pain.
If cancer has spread to the cervix, palliative treatment may be beneficial.
This type of treatment may also slow the growth of cancer.
If this happens, you should consult your doctor immediately.
Only then will your treatment plan be determined.
Besides the physical signs of stage I vulvar cancer, other symptoms of stage I vulvar cancer include bleeding, itching, and discoloration of the skin.
During this time, you should take a smear test to detect early-stage cancer.
Moreover, you should check for any changes in the color of your vaginal lip.
When cancer occurs in the vulva, it can spread to other areas of your body.

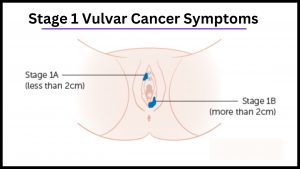
What are the Differences Between Stages 1A and Stages 1B Vulvar Cancer?
Stage IA vulvar cancer has not spread beyond the vulva.
While Stage IB has spread to the vagina and lower urethra but has not yet metastasized to lymph nodes.
Stage IA cancer is located in the vulva and perineum, the area between the vagina and rectum.
It has grown to a diameter of approximately one millimeter and has not spread to the nearby lymph nodes or distant sites.
And for Stage 1A you might not need surgery to know if cancer has spread to your lymph nodes.
Stage IB cancer, on the other hand, has grown larger and has spread to the vulva or perineum.
Also, Stage IB lesions are approximately two centimeters in diameter.
And for Stage 1B an expert will wish to check for the possibility of its spreading to your lymph nodes.
Stage II vulvar cancer has spread to distant sites and has grown to more than 2 cm in size.
A tumor in stage II is considered Stage III vulvar cancer if it has metastasized to other parts of the body, including lymph nodes.
FDG-PET is often an adjunctive test.
Its multiplanar ability and superior soft-tissue contrast make it a preferred imaging technique for vulvar cancer.
It also facilitates treatment planning.
Contrast-enhanced pelvic MRI should be used whenever possible.
Patients diagnosed with vulvar cancer should undergo the diagnostic test when it is indicated.
Andersen et al. reported on the evaluation of 27 patients with vulvar cancer, including seven patients with stage 1a and stage 1b disease and three patients with stage 0b and asymptomatic cecum.
In the United States, vulvar cancer is a relatively rare gynecologic malignancy.
The majority of patients are diagnosed at an early stage, and most tumors originate in the labia majora.
Patients with vulvar cancer have a five-year survival rate of 86% for vulvar confined disease, while survival rates drop to 57% for patients with distant metastases.
If a woman develops persistent symptoms of vulvar cancer, she should see her primary care physician or gynecologist for further evaluation.
She can also sign up for a free health newsletter that focuses on the latest information in this area.
As vulvar cancer is not completely curable, early detection can greatly improve a woman’s chances of survival.
Surgery is the principal treatment method for vulvar cancer.
The goal of surgery is to remove the entire VIN lesion while preserving the vulvar anatomy.
A simple vulvectomy has a 5-year survival rate of over 90%, but this surgical procedure is rarely recommended.
There are limited surgical techniques available, including partial vulvectomy.
These are often less invasive and less deforming.
Ultimately, the choice of treatment depends on the extent of the disease and the experience of the treating physician.
A doctor will determine the stage of vulvar cancer by analyzing the results of tests.
The stage will inform the doctor of the extent of the tumor, whether the cancer has spread to nearby organs and the prognosis.
For stage 1a vulvar cancer, doctors will need to remove the affected part of the vagina to find cancer.
The tumor will be analyzed using imaging scans.
The risk of lymph node metastases is based on the primary tumor’s size, depth of stromal invasion, and presence of lymphovascular space invasion.
Typically, vulvar carcinoma will spread via the lymphatic system to superficial and deep inguinal lymph nodes.
The pelvic lymph nodes will be involved if cancer has metastasized beyond the vulvar.
To determine the accuracy of magnetic resonance imaging in vulvar cancer, Sohaib et al. evaluated 22 patients with primary vulvar SCC with 18 unenhanced and four contrast-enhanced MRI scans.
In this study, they found that MRI correctly staged the extent of the primary tumor in seventy percent of the patients.
A similar study by Kataoka et al. evaluated 49 patients with vulvar cancer and found that the MRI was more accurate for predicting tumor size.
SLN is an excellent treatment for early-stage vulvar cancer.
A recent study conducted at the University of Texas Medical School suggested it could significantly improve the survival rate of patients who underwent surgery for vulvar cancer.
It was also associated with significant improvements in overall survival.
However, it is important to note that cancer must have spread beyond the vulva to nearby tissue.
In stage IIIB, cancer has spread to the lymph nodes of the groin.
A tumor in stage II may be any size.
In addition to the vagina, it can also spread to the anus and the urethra.
MRI of the pelvic region is considered a valid option if a tumor is large or in the lower vagina.
In stage II, the tumor may involve the urethra, pelvic bone, and inguinofemoral lymph nodes.

Stage 1 Vulvar Cancer Treatment – And what you need to Know.
Stage 1 vulvar cancer treatment options can include a surgical procedure to remove the entire affected vulva, and radiation therapy.
In some cases, chemotherapy and radiation may be combined.
If cancer has spread to lymph nodes or nearby tissues, surgery may be the only option.
However, there are certain limitations to surgery, including invasiveness.
Before undergoing this procedure, patients must discuss all options with their doctor.
After this surgery, treatment will depend on the type of cancer and the extent of the tumor.
Treatment for stage I vulvar cancer will depend on the size of the tumor, the spread of cancer, and the patient’s overall health and wishes.
Surgical procedures may be used to remove cancer while preserving normal tissue.
Laser surgery uses a laser beam to remove cancer while leaving a margin of healthy tissue around it.
And laser surgery may also be used to remove surface lesions.
Patients with stage I vulvar cancer may also undergo a surgical procedure called a wide local excision.
Many doctors will use multidisciplinary teams to treat stage 1 vulvar cancer.
The doctors in these teams make decisions about the best treatments.
They may consult a surgeon, a non-surgical oncologist, or a cancer nurse.
It can be confusing to decide which treatments are best for you, so it’s important to have a clear understanding of the options.
Your healthcare provider will discuss your treatment options and the pros and cons of each.
Surgery is another option for treatment.
Radiation therapy may help shrink the tumor and reduce symptoms.
This procedure is often done by performing a pelvic exenteration.
In this procedure, the pelvic lymph nodes, cervix, and lower colon are removed.
The surgeon may also create an artificial opening for urine to flow into a collection bag.
After the surgery, chemotherapy may be recommended.
A radiation therapy treatment may be an option if the cancer is spread to the cervix.
If a vulva tumor is in a confined area, chemotherapy or radiation therapy may be necessary.
Surgery may be an option if it has spread to nearby structures.
Stage IB cancer has spread to lymph nodes and is more than 2 centimeters long.
However, cancer that has spread to lymph nodes and nearby structures is considered stage II.
However, chemotherapy will not cure a stage IB tumor, as it will continue to spread throughout the body.
During a vulvar cancer screening, your doctor will perform a pelvic examination, which includes an inspection of the cervix, fallopian tubes, uterus, and rectum.
Your doctor may also perform a biopsy to check for tumor spread or to determine if there is any evidence of cancer spread.
Imaging scans may also be necessary, including X-rays.
For stage 1 vulvar cancer treatment, the physician should consider several options to treat your condition.
In stage 1, chemotherapy is the most common treatment option.
This procedure is used to shrink the vulvar tumor and preserve urinary and bowel function.
In combination with radiation therapy, chemotherapy is administered concurrently with radiation therapy.
This treatment is also called chemoradiation therapy.
It is usually given in the same session as radiation therapy to maximize the effectiveness of both approaches.
In addition, chemotherapy may be combined with radiation therapy, depending on the location and type of cancer.

Stage 1 Vulvar Cancer Survival Rate – What is the Survival Rate?
The survival rate for stage 1 vulvar cancer depends on the tumor’s depth.
In this study, patients with a depth of 2 mm had a survival rate of 71%, while patients with a depth of one mm had a survival rate of 50%.
However, survival rates were worse for patients with deeper tumor invasion, as evidenced by the Kaplan-Meier survival curve.
The most successful surgical methods were vulvectomy, bilateral lymphadenectomy, and hemivulvectomy.
But these treatments are not the only ones available.
It is not easy to predict the survival rate of stage 1 vulvar cancer.
The first step is to find out if cancer has spread to distant areas.
Also, the stage of vulvar cancer is determined by a number of factors, including size, location, and tumor stage.
Stage 1 indicates that the cancer is localized, and stage 4 signifies that it has spread to distant areas.
Fortunately, the overall survival rate for stage 1 vulvar cancer is very high.
Currently, 86 percent of women will survive vulvar cancer if detected early.
In contrast, the survival rate of stage 3 cancer is only 18 percent.
Also, in the United States, vulvar cancer is not common, and only makes up a small portion of all cancers in women.
Several factors influence the survival rate of vulvar cancer.
The stage at which the cancer is detected is also important.
Also, the survival rates for stage 1 vulvar cancer vary according to the stage and grade of the disease.
The survival rates are based on data collected from SEER 12 and the U.S. Mortality Database.
Also, the rates were calculated using Joinpoint Trend Analysis Software.
The data was collected from the years 2015-2019.
It is important to remember that vulvar cancer can spread, so an early diagnosis is critical.
In addition to early detection, you should also seek a physician if you notice any changes in the vulvar area.
Fortunately, the survival rate for stage 1 vulvar cancer is very high.
Stage 0 vulvar cancer is a relatively mild form of cancer and can be removed with minimal surgical intervention.
Unlike stage I, stage 0 cancer has not spread to distant organs.
By stage III, cancer has reached lymph nodes and is embedded in the lower third of the vagina.
It may also spread to the anus and pelvic organs.
Although the mortality rate for stage 1 vulvar cancer is low, the survival rate for patients with the disease depends on several factors.
The treatment, lymphadenectomy, lymphadenectomy, and surgical staging are all important factors in determining the survival rate.
And the cancer stage will also determine how large the resection margins should be.
Surgical treatments for vulvar cancer may be successful in preventing cancer from returning.
Currently, individualized treatment is recommended for early-stage vulvar cancer patients.
This approach helps reduce morbidity and complications after inguinal lymphadenectomy.
Additionally, individualized treatments have been shown to decrease the number of patients who develop groin recurrence.
Inguinal radiation may be an effective treatment option for stage 1 vulvar cancer.
However, there are still a number of complications related to surgery.

Premalignant Finding.
Women with a family history of vulvar cancer or dysplastic nevi have an increased risk for vulvar cancer.
People with certain immune system diseases, such as HIV, are also at risk.
Also, people who are overweight and have diabetes have a greater risk for vulvar cancer.
However, no one knows what exactly causes vulvar cancer, or why some women develop it.
Knowing the risk factors can help you make better health care and lifestyle decisions.
If you have vulvar cancer or a premalignant finding, you may be eligible for surgery to remove the affected area.
This procedure can remove the affected area and the normal tissue surrounding it so that all precancer cells are removed.
There are also some treatment options that involve removing the cancerous cells, including laser treatments and topical medicines.
Some of these treatments include fluorouracil (5-FU) and imiquimod, which can be applied to the vulva.

Can Stage 1 Vulvar Cancer Be Cured?
There are several treatment options for Stage 1 vulvar cancer.
Surgery is the most common procedure, but other options include Chemotherapy, Skin grafts, and Lymphadenectomy.
If you are diagnosed with Stage 1 vulvar cancer, you should know that the outlook is good if you receive treatment early.
However, the disease is likely to spread if it is not treated quickly.
Symptoms of vulvar cancer can include a lump or ulceration, itching, irritation, bleeding, and ulceration in the vulvar area.
You should visit a doctor if you notice any changes in the area.
The early diagnosis of this condition will greatly improve your outlook.
Surgery
Surgical treatment for vulvar cancer is always successful.
While some cases of vulvar cancer are cured with surgery, others require additional treatments.
Depending on the stage of the disease, a lymph node dissection or sentinel lymph node biopsy may be needed.
This surgery removes lymph nodes from one or both sides of the groin.
It also involves chemotherapy and radiotherapy.
Chemotherapy
Patients who have stage I vulvar cancer typically have two treatment options: surgery or chemotherapy.
Surgery is an excellent choice if cancer has not spread to surrounding lymph nodes, but may be required in the event of a recurrence.
Chemotherapy is also an option in some cases, although it should not be used in cases of stage II vulvar cancer.
In addition to surgery, some patients also undergo radiotherapy or chemotherapy, depending on the stage and type of cancer.
Skin grafts
Most women with vulvar cancer experience itching, burning, and other symptoms long before the appearance of a lump.
Unfortunately, this type of cancer is sometimes misdiagnosed as a yeast infection and treated with ineffective creams.
Because it occurs in both men and women, it is not uncommon for women to experience a medical condition that is closely related to vulvar cancer.
Lymphadenectomy
The prognosis of patients with Stage 1 vulvar cancer can be influenced by their surgical approach, but the exact role of lymphadenectomy in the prognosis is not clear.
Patients who underwent en bloc vulvar lymphadenectomy with wide local excision have a higher five-year survival rate than patients who underwent pelvic lymphadenectomy alone.
Palliative care
Palliative care refers to treatments and services that improve a person’s quality of life and minimize pain and suffering associated with a cancer diagnosis.
It can be helpful in any stage of vulvar cancer, whether it’s stage 1 or stage 4.
Palliative care for vulvar cancer can help reduce symptoms and slow the progression of the disease.
However, it must be determined which treatments are right for you.

How Fast Does Vulvar Cancer Spread?
You may be wondering how fast vulvar cancer spread.
The stage of cancer will indicate the extent of the disease and whether it will spread to other parts of the body.
FIGO, the International Federation of Obstetrics and Gynecology, has developed different stages.
Doctors assign the stage of cancer based on the size of the tumor and whether it has spread to other parts of the body.
In addition to the cancer stage, doctors will consider tumor grade and location.
The type of operation a patient receives will depend on the stage of vulvar cancer and how advanced it is.
Surgery, chemotherapy, and radiation therapy are among the options available.
Each type of treatment has its own set of risks and side effects, so your doctor will discuss them with you prior to recommending any treatments.
Surgical treatment for vulvar cancer usually involves surgical removal of the tumor.
The doctor will determine which type of surgery is best for your case and discuss the risks and benefits of each.
In addition to surgical procedures, a patient will need to undergo diagnostic tests to determine the stage of their cancer.
Often, a healthcare provider will use imaging scans and CTs to determine the stage.
These tests are essential for determining the correct treatment plan.
If a patient has no symptoms or has symptoms but is experiencing pain, surgery is an option.
Once treatment is decided upon, the patient will be treated accordingly.
In addition to surgical treatment, women with vulvar cancer may undergo chemotherapy, which includes high-energy rays aimed at the cancer to shrink it.
These rays are targeted by a machine outside the body.
While most side effects subside after the treatment is complete, some may remain long-term.
Treatments with chemotherapy can lead to skin soreness, and some patients may even be radioactive.
Surgery to remove the tumor is the most common treatment for vulvar cancer.
While it can be successful, there are risks to a woman’s vulva, including infection, bleeding, blood clots, and altered sensation during sex.
Additionally, if a woman has lymph node involvement, additional groin surgery may be required.
A woman may be unable to drive or lift heavy objects for six to eight weeks after surgery.
However, the recovery process will be quicker with proper rest and gentle exercise.
Stage III is one of the most advanced stages of vulvar cancer.
The tumor has spread beyond the vulva to nearby tissues such as the anus and urethra.
In this stage, cancer has spread to nearby lymph nodes but not yet too distant areas.
It may have spread to nearby lymph nodes and distant organs.
In this stage, it may be difficult to detect cancer.
But, it is important to remember that it will likely spread to nearby tissues and lymph nodes before the cancer is diagnosed in the vulva.
A patient with vulvar cancer recently developed a local recurrence after treatment for vulvar SCC.
In September 2017, the patient developed a 3 cm nodule in the right vulvar and a 0.8 cm lesion in the clitoris.
A vulvar SCC has a poor prognosis if it has spread to distant organs.
Despite its rarity, vulvar SCC can spread lymphatically, and the lymphatic spread involves the ipsilateral inguinal and femoral lymph nodes.
Moreover, lymphatic spread is the single most common form of the disease, and patients with lymph node involvement have a better prognosis.
For women who have nodal involvement, the 5-year overall survival rate is higher than ninety percent of patients.
Conclusion:
When women suspect that they have vulvar cancer, they are often confused about the signs and symptoms of stage 1 disease.
However, there are many signs and symptoms that indicate that they may have stage 1 cancer.
By following a few simple steps, you can easily detect the early stages of vulvar cancer and seek treatment.
Listed above are some common symptoms that can indicate that you may have stage 1 vulvar cancer.
Your doctor may order imaging tests to confirm whether you have vulvar cancer.
These tests may include a TC scan, MRI, or an X-ray.
Depending on the size of the tumor, imaging tests may also indicate if it has spread to nearby tissues, such as the lungs.
The extent of cancer’s spread will also determine the stage of treatment.
Your doctor will also use the imaging results to decide on your treatment options.
A dark patch of discoloration may be the first sign of vulvar cancer.
Symptoms of this disease can be indicative of other conditions as well.
For example, your doctor might suspect a bacterial infection or a virus infection.
While you may have vulvar melanoma, you may not have one.
Other possible conditions include adenocarcinoma and sarcoma.
Verrucous carcinoma, a subtype of squamous cell cancer, may look like a wart.
Although most types of vulvar cancer are not life-threatening, they should be treated as early as possible.
Early diagnosis improves your chances of survival.
Even if you do have stage 1 vulvar cancer, treatment is possible.
Treatment is the key to survival.
In the event that the condition does not progress, the disease can spread throughout the body and cause complications.
Your doctor will perform a physical exam and ask questions to rule out other causes of the disease.